How to Interpret a Prostate Biopsy Report
Hey Dr. Jafri, I had a prostate biopsy done, can you walk me through my prostate biopsy results?
Sure, let’s do this. There is a ton of information in a prostate biopsy report and let me walk you through how I go over this with my patients. Once we go over this in a systematic way, I think you will have a better understanding of what is going on and what to look for going forward. Off we go!
The #1 question on your mind and first one to ask--Is there cancer or not?
The first thing that you will hear is whether the prostate biopsy showed cancer or not. This is the answer to the question that we have been waiting for.
Your urologist will hopefully say that the biopsy is BENIGN. Benign means that there is no cancer tissue seen. HOORAY.
On the other hand, the urologist may say the biopsy showed a MALIGNANCY. This means that the results showed cancer 🙁.
Now, here is another confusing, but possible scenario. The urologist may say that the biopsy results was neither benign nor malignant. Huh? What could that mean?
There are two other possibilities that the biopsy could show. It can also potentially show HIGH-GRADE PROSTATIC INTRAEPITHELIAL NEOPLASIA (HGPIN) or ATYPICAL SMALL ACINAR HYPERPLASIA (ASAP). Let’s talk about these separately.
For HGPIN, it matters about the number of cores involved. If there was only one sample that showed this, then no worries, your prostate biopsy is the same as one that has no cancer. If there were multiple cores of HGPIN or if the biopsy showed ASAP, then the urologist will recommend a repeat biopsy as there is a possibility that there was cancer that was missed.
What should I expect my urologist to review next if it did show cancer?
There are a lot of details within the biopsy report and this will really really help guide your treatment options. For prostate cancer, one of the most difficult aspects of coming up with a treatment plan is that there are choices. It’s sometimes easier when there is only one option but oftentimes there are multiple excellent treatment choices that you can fall back on. If you want more details about choosing between surgery or radiation for prostate cancer, then click over here.
I am going to walk through how I review a biopsy report with my patients who have been diagnosed with cancer.
Grade Group or Gleason Score
In general, prostate cancer is called ‘adenocarcinoma of the prostate’. Almost all prostate cancers fit within this cell type and the focus of this post will be to review this.
The pathologist will look at the samples of tissue and how the cells are arranged and give it two scores. The primary pattern that they see will be given the first score and the second most common pattern they see will be given the second score. These patterns will be graded 1-5 with five being the most serious. These numbers are then added up to give a ‘score’. The lowest score that we call prostate cancer is a six and the highest score is a ten and this is your GLEASON SCORE.
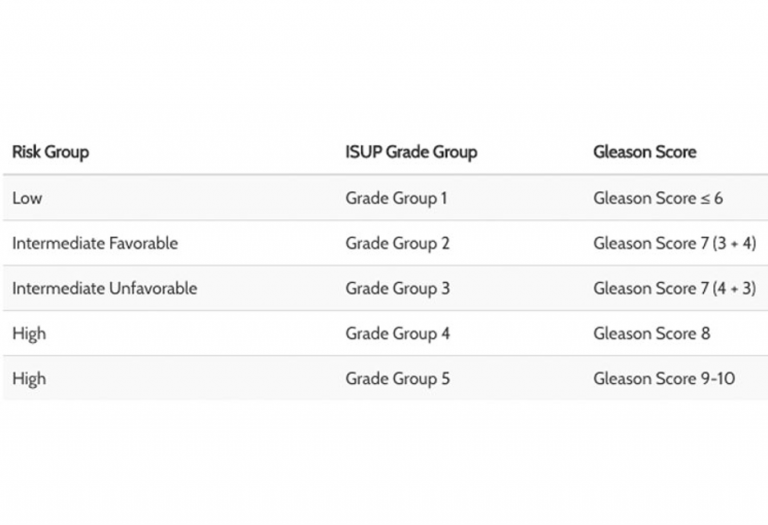
Let’s walk through an example. When we see a result that says 3+4=7, the pathologist is saying that the most common pattern is a 3 and the second most common pattern is a 7. So then we add up those two numbers and will tell you that you have “Gleason 3+4=7 prostate cancer”. Now, Gleason 3+4=7 is less aggressive than 4+3=7 and that is why many have started to adopt a newer system to rate people as below:
Number of prostate biopsy cores involved
During the biopsy, the urologist will have taken several samples, or cores, from the prostate. This was done with a prostate specialized device that went through the ultrasound probe and removed a small sample of the prostate tissue. This tissue comes out looking like a silk worm. The number of these cores that are positive will play into your disease risk.
The more the number of cores involved, the more concerning.
The percent core volume of tissue involved
Not only is the number of cores involved important, but the percent involvement of the core is important as well. The aggressiveness of the cancer is deemed differently if only 5% of the sample showed cancer versus 75%. This becomes important when seeing your eligibility for certain treatment options such as active surveillance.
Discuss prognosis of your cancer
With the biopsy report, there is now a LOT of information to process and interpret. There are numerous risk calculators, or nomograms, that can further help provide information to help understand the overall burden of your cancer.
These nomograms will often taken into account your age, PSA level, rectal exam findings, and biopsy report. These nomograms will spit out information ranging from your overall survival to the likelihood the cancer has spread to the lymph nodes or beyond. These help to kind of recap all the details of your situation and give you a better understanding of your new diagnosis.
So based on this, what is my “stage”?
For prostate cancer, I will actually use a different terminology: very low, low, intermediate and high risk. This really helps us to determine what treatment options are available. See below for how the risk groups are organized by NCCN Guidelines.
Very Low risk
- Normal prostate exam (clinical T1c)
- Gleason Score 6 (“Grade Group 1”)
- PSA < 10
- Fewer than 3 biopsy cores positive
- Less than 50% cancer in a core
- PSA density <0.15 (looking at the PSA based on the size of the prostate)
Low Risk Prostate Cancer
- Normal prostate exam (clinical T1c) or a small nodule felt
- Gleason Score 6 (“Grade Group 1”)
- PSA < 10
Intermediate Risk Prostate Cancer
- Prostate exam will feel a nodule (clinical T2b or T2c)
- Gleason Score 3+4=7 or 4+3=7 (“Grade Group 2 or 3”)
- PSA 10-20
High Risk Prostate Cancer
- Cancer felt to be just outside the prostate (clinical T3a)
- Gleason Score 8 or Gleason 9-10 (“Grade Group 4 or 5”)
- PSA >20
Very High Risk Prostate Cancer
- Really abnormal prostate exam (clinical T3b-T4)
- Primary Gleason Pattern 5 or
- >4 cores with Grade Group 4-5
Dr. Jafri's Wrapup
This is the process that I like to go over with my patients when they come back to review the results from a prostate biopsy.
I will go over if they have cancer or not. If they have cancer, I will then talk about if they need treatment or can we just monitor the cancer. This decision will be based on factors like the Gleason score, the number of cores involved, and how much cancer is in each core.
Based on this information, I will also go over prognosis. In general, people with prostate cancer do GREAT. I like to first reassure my patients that usually with whatever discussion we have, prostate cancer has many great treatment options and I will explain the pros and cons of each option. If you have been diagnosed with prostate cancer and want to see what else besides Urology Buddy could be a good resource, click over here.

Dear Dr. Jafri,
Thanks so much for a very informative read in what is a very well-written document. There is one small thing you might change, though: In line 2 of block 3 under the heading ‘Grade Group or Gleason Score,’ I think the ‘7’ should be a ‘4.’ It’s just a small point–the reader should be able to figure out what is meant–but I thought that, in the event no one had yet brought it to your attention, I would.
Again, really nice, thorough summary of a biopsy interpretation. It has helped me to understand my results a little better. My own results suggest I am at the intermediate stage (17 samples, 8 positive: one is 3+3, six are 3+4, and 1 is 4+3; PSA around 18). I am a heart patient (major heart attack–LAD blockage–in 2008; quintuple-heart bypass in 2014; hibernating myocardium since 2019 with a stent in artery feeding the 2 major coronary arteries that are still open). I am debating whether it’s worth having any treatment of my prostate cancer, given that my subjective feeling is that I will not live more than 10 more years at best. Can you recommend a good site for information on heart patients with prostate cancer?
With many thanks and wishing you a nice day,
Tim K.
So you get placed in the “unfavorable intermediate” risk category by NCCN guidelines. If you go to Chapter 6 of https://www.nccn.org/patients/guidelines/content/PDF/prostate-early-patient.pdf then you can see some blanket recommendations on someone in your situation. Not specific to a heart patient but does give context of treatment recommendations based on your life expectancy. In terms of your life expectancy as a factor in deciding, I think a formal discussion with your Cardiologist would be helpful.